Background
Gastroesophageal reflux is a normal physiologic phenomenon experienced intermittently by most people, particularly after a meal. Gastroesophageal reflux disease (GERD) occurs when the amount of gastric juice that refluxes into the esophagus exceeds the normal limit, causing symptoms with or without associated esophageal mucosal injury (ie, esophagitis).
A study by Richter and a Gallup Organization National Survey estimated that 25%-40% of healthy adult Americans experience symptomatic GERD, most commonly manifested clinically by pyrosis (heartburn), at least once a month. Furthermore, approximately 7%-10% of the adult population in the United States experiences such symptoms on a daily basis.
In most persons with GERD, endogenous defense mechanisms either limit the amount of noxious material that is introduced into the esophagus or rapidly clear the material from the esophagus so that symptoms and esophageal mucosal irritation are minimized. Examples of the defense mechanisms include actions of the lower esophageal sphincter (LES) and normal esophageal motility. When the defense mechanisms are defective or become overwhelmed so that the esophagus is bathed in acid or bile and acid-containing fluid for prolonged periods, GERD can be said to exist.
Signs and symptoms
- Typical esophageal symptoms include the following:
- Heartburn
- Regurgitation
- Dysphagia
- Abnormal reflux can cause atypical (extraesophageal) symptoms, such as the following:
- Coughing and/or wheezing
- Hoarseness, sore throat
- Otitis media
- Noncardiac chest pain
- Enamel erosion or other dental manifestations
A history of nausea, vomiting, or regurgitation should alert the physician to evaluate for delayed gastric emptying.
Atypical extraesophageal symptoms
Coughing and/or wheezing are respiratory symptoms resulting from the aspiration of gastric contents into the tracheobronchial tree or from the vagal reflex arc producing bronchoconstriction. Approximately 50% of patients who have GERD-induced asthma do not experience heartburn.
Hoarseness results from irritation of the vocal cords by the gastric refluxate and is often experienced by patients in the morning.
Reflux is the most common cause of noncardiac chest pain, accounting for approximately 50% of cases. Patients can present to the emergency department with pain resembling a myocardial infarction. Reflux should be ruled out (using esophageal manometry and 24-hour pH testing if necessary) once a cardiac cause for the chest pain has been excluded. Alternatively, a therapeutic trial of a high-dose proton pump inhibitor (PPI) can be tried.
Additional atypical symptoms from abnormal reflux include damage to the lungs (eg, pneumonia, asthma, idiopathic pulmonary fibrosis), vocal cords (eg, laryngitis, cancer), ear (eg, otitis media), and teeth (eg, enamel decay).
Diagnosis
The following studies are used to evaluate patients with suspected gastroesophageal reflux disease:
Upper gastrointestinal endoscopy/esophagogastroduodenoscopy: Mandatory
Esophageal manometry: Mandatory
Ambulatory 24-hour pH monitoring: Criterion standard in establishing a diagnosis of gastroesophageal reflux disease
Studies
Upper gastrointestinal contrast-enhanced studies are the initial radiologic procedure of choice in the workup gastroesophageal reflux disease. Plain chest radiographic findings are not useful in the evaluation of this condition, but they are helpful in assessing the pulmonary status and basic anatomy. Chest images may also demonstrate a large hiatal hernia, but small hernias can be easily missed.
Currently, no role exists for computed tomography scanning, magnetic resonance imaging, or ultrasonography in the routine evaluation of patients with reflux disease.
Atypical extraesophageal symptoms
symptoms resulting from the aspiration of gastric contents into the tracheobronchial tree or from the vagal reflex arc producing bronchoconstriction. Approximately 50% of patients who have GERD-induced asthma do not experience heartburn.
Hoarseness results from irritation of the vocal cords by the gastric refluxate and is often experienced by patients in the morning.
Reflux is the most common cause of noncardiac chest pain, accounting for approximately 50% of cases. Patients can present to the emergency department with pain resembling a myocardial infarction. Reflux should be ruled out (using esophageal manometry and 24-hour pH testing if necessary) once a cardiac cause for the chest pain has been excluded. Alternatively, a therapeutic trial of a high-dose proton pump inhibitor (PPI) can be tried.
Additional atypical symptoms from abnormal reflux include damage to the lungs (eg, pneumonia, asthma, idiopathic pulmonary fibrosis), vocal cords (eg, laryngitis, cancer), ear (eg, otitis media), and teeth (eg, enamel decay).
Management
Treatment of gastroesophageal reflux disease involves a stepwise approach. The goals are to control symptoms, to heal esophagitis, and to prevent recurrent esophagitis or other complications. The treatment is based on lifestyle modifications and control of gastric acid secretion through medical therapy with antacids or proton pump inhibitors or surgical treatment with corrective antireflux surgery.
Nonpharmacotherapy
Lifestyle modifications used in the management of gastroesophageal reflux disease include the following:
Losing weight (if overweight)
Avoiding alcohol, chocolate, citrus juice, and tomato-based products
Avoiding peppermint, coffee, and possibly the onion family
Eating small, frequent meals rather than large meals
Waiting 3 hours after a meal to lie down
Refraining from ingesting food (except liquids) within 3 hours of bedtime
Elevating the head of the bed by 8 inches
Avoiding bending or stooping positions
Pharmacotherapy
The following medications are used in the management of gastroesophageal reflux disease:
H2 receptor antagonists (eg, cimetidine, famotidine, nizatidine)
Proton pump inhibitors (eg, omeprazole, lansoprazole, rabeprazole, esomeprazole, pantoprazole)
Prokinetic agents (eg, metoclopramide)
Antacids (eg, aluminum hydroxide, magnesium hydroxide)
Surgical options
Transthoracic and transabdominal fundoplications are performed for gastroesophageal reflux disease, including partial (anterior or posterior) and circumferential wraps. Open and laparoscopic techniques may be used.
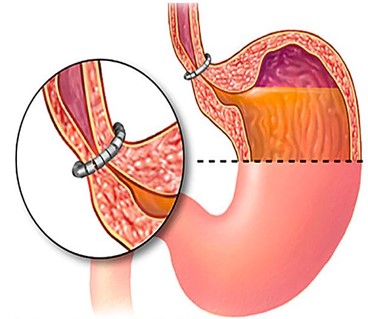
Placement of a device to augment the lower esophageal sphincter is another surgical option.
Indications for fundoplication include the following:
Patients with symptoms that are not completely controlled by proton pump inhibitors
Patients with well-controlled reflux disease who desire definitive, one-time treatment
The presence of Barrett esophagus
The presence of extraesophageal manifestations
Young patients
Poor patient compliance with medications
Postmenopausal women with osteoporosis
Patients with cardiac conduction defects
Cost of medical therapy
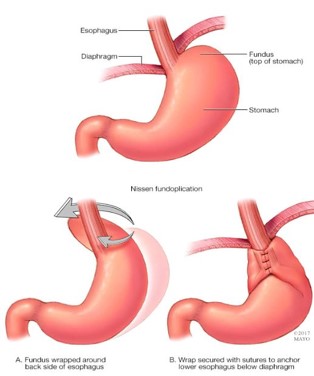
Indications for surgery (gastric fundoplication) include the following:
- Patients with symptoms that are not fully controlled by PPIs
- Patients with well-controlled reflux disease who wish a one-time definitive treatment
- Presence of Barrett’s esophagus
- The presence of manifestations outside the esophagus
- Young patients
- Impaired patient drug compliance
- Postmenopausal women with osteoporosis
- Patients with defects in cardiac conduction (electrocardiogram)
- The cost of medical treatment


